Abstract
Purpose
In general, sleeping and activity patterns vary between individuals. This attribute, known as chronotype, may affect night shift performance. In the intensive care unit (ICR), night shift performance may impact patient safety. We have investigated the effect of chronotype and social demographics on sleepiness, fatigue, and night shift on the performance of nurses.
Methods
This was a prospective observational cohort study which assessed the performance of 96 ICU night shift nurses during the day and night shifts in a mixed medical–surgical ICU in the Netherlands. We determined chronotype and assessed sleeping behaviour for each nurse prior to starting shift work and before free days. The level of sleepiness and fatigue of nurses during the day and night shifts was determined, as was the effect of these conditions on psychomotor vigilance and mathematical problem-solving.
Results
The majority of ICU nurses had a preference for early activity (morning chronotype). Compared to their counterparts (i.e. evening chronotypes), they were more likely to nap before commencing night shifts and more likely to have young children living at home. Despite increased sleepiness and fatigue during night shifts, no effect on psychomotor vigilance was observed during night shifts. Problem-solving accuracy remained high during night shifts, at the cost of productivity.
Conclusions
Most of the ICU night shift nurses assessed here appeared to have adapted well to night shift work, despite the high percentage of morning chronotypes, possibly due to their 8-h shift duration. Parental responsibilities may, however, influence shift work tolerance.
Similar content being viewed by others
Introduction
Night shift work disrupts the sleep–wake cycle and its synchrony with the body’s natural biological rhythms, which may lead to fatigue and sleepiness [1]. As sleepiness and fatigue increase, alertness decreases, problem-solving and reasoning ability become slower, psychomotor skills decline and the rate of false responses to visual stimuli increases [2–5].
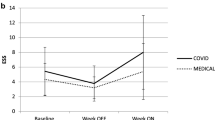
Chronotype refers to the genetic and age-dependent preference of people to specific hours of activity [6]. Generally, morning types do well in the early hours, but struggle with sleepiness relatively early (Fig. 1a) while, conversely, evening types struggle in the early hours and fare well at the end of the day. Consequently, morning chronotypes are expected to be less tolerant to night shift work than their evening counterparts [7].
The theoretical effect of chronotype on sleepiness. Sleepiness of morning chronotypes (blue) and evening chronotypes (red) is moderated by arousal systems. In this example, on free days (a), the morning chronotype naturally wakes up (sleep offset) at 0700 hours, and the evening chronotype 3 h later. From this point onward, sleepiness steadily increases (dashed line). At some point of low circadian arousal (sleep onset) sleep is enabled to reduce sleepiness. Note the difference in sleepiness between chronotypes at any given time; this is due to the phase difference of the sleep–wake cycle. During night shifts (b), sleepiness keeps increasing despite low arousal. In this example, however, the morning chronotype has a short nap at 2000 hours, which undercuts the projected sleepiness (dashed line) during the night shift. As a result, both chronotypes experience similar sleepiness during the night shift. Afterwards, both chronotypes sleep for approximately 5 h, rapidly decreasing sleepiness, but due to their misalignment with circadian arousal, they both wake up near the peak of circadian arousal
Employees with insufficient coping behaviours who are scheduled to work at times incompatible with their chronotype are more vulnerable to psychological problems [8]. Fortunately, coping strategies, such as daytime napping before a night shift, can contribute greatly to both the social and health consequences of shift work (Fig. 1, panel b) [9, 10].
The intensive care unit (ICU) is a particularly demanding working environment for medical and nursing staff, where, despite remarkable achievements in diagnostics and treatment options, variations in quality of care still occur. Diminished coping to irregular work schedules could increase the susceptibility of the healthcare giver to lapses of vigilance or judgement, possibly decreasing patient safety [11].
The long work hours of healthcare professionals have long been a subject of debate [12]. Several studies have emphasized the degradation of performance during shift work, especially when physicians and nurses are subjected to prolonged shifts [13]. Conversely, decreasing shift duration to a maximum of 16 h is associated with deteriorating perceived quality of care [14], often attributed to decreased continuity of care [13].
We hypothesize that even shorter shifts in 36-h work weeks leave time for individuals with different demographics and chronotypes to adapt to irregular shifts. This approach favours the benefits of a reduced and more evenly spread workload over a potential decline of continuity and is in contrast to the system of continuity of care with prolonged, but often exhaustingly long shifts [15, 16]. In the study reported here, we assessed the effects of chronotype and other demographics on night shift performance in a Dutch ICU where 8-h work shifts are common.
Materials and methods
Procedure and participants
Between April and May 2013, ICU nurses working day and night shifts at the University Medical Center Groningen (the Netherlands) were sent a personal link to a site containing a battery of questionnaires and tests. This method was adopted to ensure maximum participation (i.e. via desktop computers and mobile devices) and anonymous data collection. All questions, tests and tasks had been translated into Dutch. The local medical ethics committee (METc UMCG, M13.130091) reviewed and approved the study protocols, waiving the need for formal informed consent.
The web application consisted of three modules. The first module consisted of a questionnaire for relevant background information, with the Munich ChronoType Questionnaire for Shift-Workers (MCTQshift) used to determine chronotype and sleeping behaviour. The two performance modules were accessible to the nurses during two of the last 4 h of their respective shift (1400–1600 hours for day shifts and 0400–0600 hours for night shifts) and consisted of the Karolinska sleepiness scale (KSS), the Samn–Perelli Fatigue scale (SPF), a 5-min Psychomotor Vigilance Task (PVT) and a 5-min two-digit addition test (TDAT). The day shifts on the ICU of the University Medical Center Groningen generally start at 0730–0800 hours and end at 1530–1600 hours, and night shifts generally start at 2300–2330 hours and end at 0730–0800 hours, although variations in the start of shift times do occur. Those nurses who participated in the study had different shift schedules which varied in cycle length and sequence.
Participants could only use the same type of device for both performance modules to ensure comparability of results. Data were processed off-line using a commercial software package (MATLAB 2012b; The MathWorks, Inc., Natick, MA). All times of day are written in the 24-h notation.
Instruments
The Munich ChronoType Questionnaire for Shift-Workers
Sleeping behaviour and chronotype were determined using the MCTQshift, which has been shown to correlate highly with the Morningness–Eveningness Questionnaire [17], daily sleep diaries and actimetry [18]. The MCTQshift was adapted for this study for use on mobile devices by clustering and shortening specific questions. Questions addressed in the MCTQshift are those on average duration of sleep before day shifts, before night shifts, before free days, and following night shifts. Participants regularly working consecutive shifts of the same type were asked to provide information on shifts amidst similar shifts. Participants rated the average quality of sleep on a scale of 1–10 (1 being the worst sleep imaginable, 10 being the perfect period of sleep) for each period.
The mid-sleep for each shift type was calculated using sleep onset and total sleep duration (TSD), where TSD is the difference between sleep onset and sleep offset. Sleep onset is calculated by adding sleep latency time to the time of intended sleep. Mid-sleep on a free day (MSF) was corrected for the potential sleep debt during weekdays (MSFsc) in a manner analogous to the method reported by Vetter et al. [19] when the TSD on free days exceeded the TSD on the average working day. A MSFsc of 0330 separated morning chronotypes from their evening counterparts [7].
Due to inter-individual differences in sleep need, we calculated the relative sleep duration by dividing TSD by sleep need, where sleep need was the weighted average TSD for each shift type and free days.
Wittmann et al. [20] coined the term ‘social jetlag’ to quantify the discrepancy between sleep on a working day and sleep on a free day, defined as the difference between mid-sleep on a working day and MSF. Evening chronotypes may in particular experience sleep debt due to the constraints of morning shifts, since their sleep times are shifted from their preferred times. Positive jetlag means that sleep times are brought forward; negative jetlag indicates a delay of sleep times.
Karolinska Sleepiness Scale
The KSS is a subjective scale used to measure sleepiness on a scale ranging from 1 to 9, with 1 = very alert; 3 = alert; 5 = neither alert nor sleepy; 7 sleepy, but no effort to keep awake; 9 = very sleepy great effort to keep awake [21].
Samn–Perelli fatigue scale
The SPF scale provides a subjective measure of fatigue on a scale ranging from 1 to 7, with 1 = fully alert; wide awake; 2 = very lively, responsive, but not at peak; 3 = okay, somewhat fresh; 4 = a little tired, less than fresh; 5 = moderately tired, let down; 6 = extremely tired, very difficult to concentrate; 7 = completely exhausted, unable to function effectively [22].
Psychomotor vigilance task
The PVT is a sustained-attention task which measures simple reaction time (RT) to a visual stimulus and counts the number of lapses [23]. It has been validated for assessment of neurocognitive performance in a number of studies [24–27]. In this task, the participant is asked to press a button on a keyboard, mouse or touchscreen when a grey button on the screen turns red. This stimulus is given randomly every 2–10 s, and the RT is stored. After a reaction or after 5 s of absence of reaction, the stimulus ends, and the timer for the next stimulus is reset. RTs of >750 ms are considered to indicate attention failure and are characterized as a lapse of attention. In our study, the PVT was limited to 5 min.
Two-digit adding test
To measure quick problem-solving performance, we asked our participants to perform a TDAT. In this test, the participant is presented with the task of adding together two random double-digit numbers giving the correct answer. After confirming the chosen answer by pressing a button on the screen, the next addition task is immediately presented; this process is repeated for 5 min. The participant is asked to correctly solve as many problems as possible within this 5-min window. The percentage of correct answers and the time taken per problem are stored, as is the percentage of lapses (RT > 10 s).
Statistics
For the analysis of PVT and TDAT data, we calculated the values below which 50, 15 and 85 % of RTs were found [i.e. the 50th percentile (RT50 %), 15th percentile (RT15 %) and 85th percentile (RT85 %) respectively]. Two-tailed t tests were used to compare means between groups, such as between chronotypes and shift types, when data were normally distributed. For other distributions, the Mann–Whitney U test was performed. Paired t tests determined significance of the difference between day-shift and night-shift performances, which were all normally distributed. The Kolmogorov–Smirnov one-sample test was applied to test for violation of normal distribution.
Results
Study population
A total of 96 (25 male, 71 female) ICU nurses completed the questionnaires and tests, including the MCTQshift. The results of their chronotype analysis are given in Table 1, and an overview of individual sleep times derived from the MCTQshift is given in Fig. 2. Participants were predominantly morning types (n = 61, 64 %), with a MSFsc of 03:06 ± 1:05 hours:minutes. The distribution of age was bimodal for both chronotypes, with similar means. Morning chronotypes were more than twofold more likely than evening chronotypes to have young children living at home (38 vs. 14 %, respectively; p = 0.0148) and to sleep shortly before beginning a night shift, but not more likely to sleep shortly after completion of a night shift. Similar numbers of morning and evening chronotypes frequently took naps after completion of a day shift, when working night shifts and on free days. Participants were not able to nap when working day shifts due to current ICU behavioural norms.
Sleep times for individual nurses. Sleep onset, offset and mid-sleep times for all 96 participants are displayed for free days (a), sleep before day shifts (b) and sleep before and after night shifts (c). Individual lines represent sleep duration on an average day with the specified shift, starting at sleep onset and ending at sleep offset, dots on lines represent mid-sleep times. Participants are sorted by their MSFsc (a). The horizontal dotted line separates morning (blue) from evening (red) chronotypes. Note that three participants regularly started day shifts much later than the rest of the cohort
The Therapeutic Intervention Scoring System (TISS-28) scores of all patients combined were similar for day and night shifts (combined TISS: 401.52 and 402.40 points, respectively; p = 0.9512). Staffing was higher for day shifts than for night shifts (patients per nurse 0.92 and 1.26, respectively; p < 0.0001), and there were more admissions than during the night shifts (new admissions 5.20 and 0.95 new patients, respectively; p < 0.0001).
Sleep quality
Participants experienced the highest quality of sleep on free days, with a mean score of 7.71 ± 1.05. The mean quality of sleep score before starting a day shift or a night shift was significantly lower: 7.00 ± 1.26 (p < 0.0001) and 7.02 ± 1.40 (p < 0.0001), respectively. The lowest score for quality of sleep was for sleep after the night shift: 6.21 ± 1.78 (p < 0.0001). No significant differences in sleep quality between chronotypes were found (Table 2).
Mid-sleep time
A similar percentage of morning and evening chronotypes went to sleep shortly after completing the night shift. Morning chronotypes slept earlier before starting the day and night shifts than evening chronotypes. Consequently, morning chronotypes experienced virtually no social jetlag before starting day shifts, while evening chronotypes forwarded sleep times by more than 1 h. Morning chronotypes delayed their sleep more than evening chronotypes before working the night shift and shortly after completing the night shift.
Sleep duration
Both chronotypes got less sleep before starting a day shift and following a night shift than before a free day. Morning chronotypes achieved a higher percentage of their sleep need before starting a day shift than their evening counterparts, but took shorter naps before starting a night shift. Since morning and evening chronotypes had similar sleep need, morning chronotypes achieved less of their sleep need by sleeping right before a night shift than evening chronotypes.
Performance
Of the 96 participants who completed the questionnaire module, 42 (27 morning chronotypes, 15 evening chronotypes) provided insight into performance during the day and night shifts (Table 3). Based on these data, both sleepiness and fatigue increased significantly when working night shifts (by 1.40 and 0.69 points, respectively; p < 0.0001). Performance indices showed no difference in psychomotor vigilance, except for the 85th percentile of response times, which was higher during the night shift than during the day shift. The TDAT showed a high accuracy of mathematical problem-solving at the end of both the day and night shifts (i.e. percentage of correct answers), although productivity declined, reflected by increasing RTs and lower number of correctly answered problems. The occurrence of lapses also increased during night shifts. Both chronotypes exhibited similar effects of night shift work on psychomotor performance, accuracy and efficiency of mathematical problem-solving accuracy and subjective scores for sleepiness and fatigue (i.e. no significant differences between chronotypes; results not shown).
Discussion
To our knowledge, this is the first study to determine the chronotype of ICU nurses and its effect on performance during day and night shifts. We observed a clear difference between chronotypes in sleeping behaviour before and after night shifts, but not in performance, despite significant increases in fatigue and sleepiness and significant social jetlag. It would appear that adherence to normal shift durations allows all chronotypes to adapt to night shift work, by napping before and incidentally between shifts, thereby alleviating the effects of fatigue and sleepiness.
Interestingly, morning chronotypes were more likely to have young children (≤12 years of age) living at home. These children are often dependent on parents for supervision and transportation to school (pre-high school age), suggesting that young children limit the ability to sleep at preferred times, which conceivably also impacts quality of sleep. However, the difference in quality of sleep on free days between those ICU nurses with and without young children did not reach significance, possibly due to the limited sample size. Morning types also made significantly more use of the available time during the day to sleep right before starting a night shift.
Ayas et al. [28] associated extended work duration and night shift work with an increased risk of percutaneous injuries in young physicians, citing lapses of concentration and fatigue as the most contributing factors. In another study of >5,000 nurse shifts, the risk of making errors increased threefold when shifts exceeded 12.5 h and almost doubled when a work week exceeded 40 h [29]. In a recent survey of >30,000 nurses in 12 European countries, nurses working longer shifts (≥12 h) reported a lower quality of care and lower patient safety than those working ≤8 h per shift [30]. Laboratory studies have demonstrated that sleep deprivation and misalignment of circadian phase are each separately associated with frequent lapses of attention and increased RT [2, 3]. It is therefore encouraging that our sample of ICU nurses working 8 h shifts did not show increased lapses of attention during night shifts. It is possible that while working outside diurnal preferences is unavoidable, adverse side effects can be compensated by preventive napping, sleeping right before starting on the night shift, and sacrificing speed.
To increase participation in the study, night shift questionnaires were available 2 h before the day shift questionnaires relative to the start of the shift, corresponding with periods of relatively low workloads on nurses. This may have had modulating effect on the results by overestimating true end-of-shift performance during the night. Our study initially focussed on a cross-section of all ICU staff, but insufficient numbers of doctors participated. The resulting focus on nurses may reduce generalizability of our results. Nurses are however the ‘eyes and hands’ of the ICU and the first line of detection and intervention in patient wellbeing. The real-world performance of this group in particular relies heavily on vigilance and quick problem-solving accuracy, the main performance parameters of this study.
Notably, median RTs for the PVT were relatively high, even compared to previous results obtained after a similar number of hours awake [2, 19], potentially due to the delay inherent to touchscreen interfaces or the lack of continuous motivation and guidance during the experiment. We found no significant difference in average RT between touchscreen and non-touchscreen devices. Of the 96 participants, 42 finished the battery of performance tests. Although this number exceeds previous investigations of night shift performance [19, 31], participation could perhaps have been higher if a more supervised and controlled, but less practical method had been used to assess performance. Furthermore, we found no significant differences in demographical characteristics or sleep times between those who finished the battery of performance tests and those who did not.
The TDAT focusses on the ability to solve simple mathematical problems, simulating tasks such as calculation of medication doses and fluid balances or changing settings for mechanical ventilation. Precision remained unchanged during the night shifts, although responses were significantly slower during the night shift for both chronotypes. During the TDAT, participants seemed to consciously take more time checking an answer before submitting the response or simply took longer to respond.
The 5-min versions of the PVT and TDAT caused minimal interference with a normal workflow, and the automated instruction aided in easy parallel participation, at the cost of direct motivation of participants. We did not measure the effects of night shift work on the incidence of medical errors or other practical outcomes, which could be viewed as a limitation. According to a meta-analysis by Philibert [13], clinical performance is more susceptible to the effects of delayed sleep than vigilance. This is in line with our finding that vigilance did not change among our participants during the night shift, while mathematical problem-solving did. Future investigation of relative night shift performance should therefore include practical patient care-related scenarios.
Some studies suggest that evening chronotypes struggle disproportionally with early shifts, making evening shifts perhaps more suited as a neutral reference than day shifts [19]. Day shifts have also been associated with an increased risk for adverse events, although this may not be caused by fatigue or sleepiness, but rather by the increased load of diagnostic and therapeutic activities during the day [32]. Both staffing and the number of new admissions were lower during the night shift, while the number of patients remained the same. Combined, this may have influenced fatigue, notably without resulting in alarming performance degradation. Work load is hard to assess in these situations, and TISS scores do not reflect workload for individual shifts. Regretfully, alternative scoring systems were not implemented at the time of this study [33].
The adaptation of the MCTQshift used in this study focused on the first period of sleep before or after a work shift or a free day, foregoing an exact definition of such a period. This resulted in only partial information on the amount of sleep during the average work day, possible underestimating sleep need. Furthermore, most participants repeated shifts several times, but due to the large variation in work schedules we were unable to practically correct for the number, length and type of the previous shift.
Conclusion
In conclusion, we did not find a decline in vigilance or problem-solving accuracy for either chronotype among our ICU nursing cohort, possibly due to the 8-h shift duration. Problem-solving productivity was reduced during night shifts. The participating nurses seemed to adequately adapt to night shift work by sleeping shortly before and after their shift, and by napping during night shifts. This is especially true for those who are expected to struggle with night shift work due to their chronotype. The aim of future research efforts should be to quantify the effects of different approaches to irregular work shifts on real-world performance, particularly those of long and short shifts.
Abbreviations
- KSS:
-
Karolinska sleepiness scale
- MCTQshift :
-
Munich chrono type questionnaire for shift-workers
- MSF:
-
Mid-sleep on a free day
- MSFsc :
-
MSF corrected for sleep debt
- PVT:
-
Psychomotor vigilance task
- RT:
-
Response time
- RT n % :
-
nth percentile of RT
- SPF:
-
Samn–Perelli fatigue scale
- TDAT:
-
Two-digit addition test
- TISS-28:
-
Therapeutic Interventions Scoring System-28
- TSD:
-
Total sleep duration
References
Akerstedt T, Wright KP (2009) Sleep loss and fatigue in shift work and shift work disorder. Sleep Med Clin 4:257–271. doi:10.1016/j.jsmc.2009.03.001
Belenky G, Wesensten NJ, Thorne DR et al (2003) Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res 12:1–12. doi:10.1046/j.1365-2869.2003.00337.x
Wimmer F, Hoffmann R, Bonato R, Moffitt A (1992) The effects of sleep deprivation on divergent thinking and attention processes. J Sleep Res 1:223–230. doi:10.1111/j.1365-2869.1992.tb00043.x
Josten EJC, Ng-A-Tham JEE, Thierry H (2003) The effects of extended workdays on fatigue, health, performance and satisfaction in nursing. J Adv Nurs 44:643–652. doi:10.1046/j.0309-2402.2003.02854
Mohren DCL, Jansen NWH, Kant IJ et al (2002) Prevalence of common infections among employees in different work schedules. J Occup Environ Med 44:1003–1011. doi:10.1097/00043764-200211000-00005
Gander P, Signal L (2008) Who is too old for shift work? Developing better criteria. Chronobiol Int 25:199–213. doi:10.1080/07420520802077556
Roenneberg T, Wirz-Justice A, Merrow M (2003) Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms 18:80–90. doi:10.1177/0748730402239679
Härmä MI, Ilmarinen JE (1999) Towards the 24-h society–new approaches for aging shift workers? Scand J Work Environ Health 25:610–615. doi:10.5271/sjweh.488
Smith CS, Robie C, Folkard S et al (1999) A process model of shiftwork and health. J Occup Health Psychol 4:207–218. doi:10.1037/1076-8998.4.3.207
Härmä M, Knauth P, Ilmarinen J (1989) Daytime napping and its effects on alertness and short-term memory performance in shiftworkers. Int Arch Occup Environ Health 61:341–345. doi:10.1007/BF00409390
Wachter RM, Pronovost P, Shekelle P (2013) Strategies to improve patient safety: the evidence base matures. Ann Intern Med 158:350–352. doi:10.7326/0003-4819-158-5-201303050-00010
Peets A, Ayas NT (2012) Restricting resident work hours: the good, the bad, and the ugly. Crit Care Med 40:960–966. doi:10.1097/CCM.0b013e3182413bc5
Philibert I (2005) Sleep loss and performance in residents and nonphysicians: a meta-analytic examination. Sleep 28:1392–1402. doi:10.1016/S8756-3452(08)70481-X
Desai SV, Feldman L, Brown L et al (2013) Effect of the 2011 vs 2003 duty hour regulation-compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med 173:649–655. doi:10.1001/jamainternmed.2013.2973
Richardson A, Turnock C, Harris L et al (2007) A study examining the impact of 12-h shifts on critical care staff. J Nurs Manag 15:838–846. doi:10.1111/j.1365-2934.2007.00767.x
McGettrick KS, O’Neill MA (2006) Critical care nurses—perceptions of 12-h shifts. Nurs Crit Care 11:188–197. doi:10.1111/j.1362-1017.2006.00171.x
Zavada A, Gordijn MCM, Beersma DGM et al (2005) Comparison of the munich chronotype questionnaire with the Horne-Ostberg’s morningness-eveningness score. Chronobiol Int 22:267–278. doi:10.1081/CBI-200053536
Juda M, Vetter C, Roenneberg T (2013) The munich chronotype questionnaire for shift-workers (MCTQShift). J Biol Rhythms 28:130–140. doi:10.1177/0748730412475041
Vetter C, Juda M, Roenneberg T (2012) The influence of internal time, time awake, and sleep duration on cognitive performance in shiftworkers. Chronobiol Int 29:1127–1138. doi:10.3109/07420528.2012.707999
Wittmann M, Dinich J, Merrow M, Roenneberg T (2006) Social jetlag: misalignment of biological and social time. Chronobiol Int 23:497–509. doi:10.1080/07420520500545979
Akerstedt T, Gillberg M (1990) Subjective and objective sleepiness in the active individual. Int J Neurosci 52:29–37. doi:10.3109/00207459008994241
Samn SW, Perelli LP (1982) Estimating aircrew fatigue: a technique with application to airlift operations. USAF School of Aerospace Medicine Technical Report Number SAM-TR-82-21
Powell JW, Dinges DF (1985) Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav Res Methods Instrum Comput 17:652–655. doi:10.3758/BF03200977
Graw P, Kräuchi K, Knoblauch V et al (2004) Circadian and wake-dependent modulation of fastest and slowest reaction times during the psychomotor vigilance task. Physiol Behav 80:695–701. doi:10.1016/j.physbeh.2003.12.004
Wyatt JK, Ritz-De Cecco A, Czeisler CA, Dijk DJ (1999) Circadian temperature and melatonin rhythms, sleep, and neurobehavioral function in humans living on a 20-h day. Am J Physiol 277:R1152–R1163
Van Dongen HPA, Baynard MD, Maislin G, Dinges DF (2004) Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep 27:423–433
Wyatt JK, Cajochen C, Ritz-De Cecco A et al (2004) Low-dose repeated caffeine administration for circadian-phase-dependent performance degradation during extended wakefulness. Sleep 27:374–381
Ayas NT, Barger LK, Cade BE et al (2006) Extended work duration and the risk of self-reported percutaneous injuries in interns. J Am Med Assoc 296:1055–1062. doi:10.1097/01.AOG.0000252305.52668.c0
Rogers AE, Hwang W-T, Scott LD et al (2004) The working hours of hospital staff nurses and patient safety. Health Aff 23:202–212. doi:10.1377/hlthaff.23.4.202
Griffiths P, Dall’Ora C, Simon M et al (2014) Nurses’ shift length and overtime working in 12 European countries: the association with perceived quality of care and patient safety. Med Care 52:975–981. doi:10.1097/MLR.0000000000000233
Lingenfelser T, Kaschel R, Weber A et al (1994) Young hospital doctors after night duty: their task-specific cognitive status and emotional condition. Med Educ 28:566–572
Tibby SM, Correa-West J, Durward A et al (2004) Adverse events in a paediatric intensive care unit: Relationship to workload, skill mix and staff supervision. Intensive Care Med 30:1160–1166. doi:10.1007/s00134-004-2256-y
Debergh DP, Myny D, Van Herzeele I et al (2012) Measuring the nursing workload per shift in the ICU. Intensive Care Med 38:1438–1444. doi:10.1007/s00134-012-2648-3
Acknowledgments
We thank all staff of the ICU of the UMCG who participated in the study, and L. de Jong and A.D. Hunderman for their support in setting up this study. We thank F. Doesburg for his advice on figure editing and Forion Secure Web & App for building the web-application. This study was partially funded through Dialoog UMCG, an initiative to stimulate sustainable employability.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Diminished coping to irregular work schedules could increase susceptibility to lapses of vigilance or judgement, possibly decreasing patient safety during the night shift. Working 8-h shifts may negate these adverse effects, by enabling individuals with diminished coping to shift sleep times and to nap preventively.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Reinke, L., Özbay, Y., Dieperink, W. et al. The effect of chronotype on sleepiness, fatigue, and psychomotor vigilance of ICU nurses during the night shift. Intensive Care Med 41, 657–666 (2015). https://doi.org/10.1007/s00134-015-3667-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3667-7