Abstract
Objective: To investigate the effects of ambulant myofeedback training including ergonomic counselling (Mfb) and ergonomic counselling alone (EC), on work-related neck-shoulder pain and disability. Methods: Seventy-nine female computer workers reporting neck-shoulder complaints were randomly assigned to Mfb or EC and received four weeks of intervention. Pain intensity in neck, shoulders, and upper back, and pain disability, were measured at baseline, immediately after intervention, and at three and six months follow-up. Results: Pain intensity and disability had significantly decreased immediately after four weeks Mfb or EC, and the effects remained at follow up. No differences were observed between the Mfb and EC group for outcome and subjects in both intervention groups showed comparable chances for improvement in pain intensity and disability. Conclusions: Pain intensity and disability significantly reduced after both interventions and this effect remained at follow-up. No differences were observed between the two intervention groups.
Similar content being viewed by others
Introduction
Work-related musculoskeletal complaints in the upper extremity are common among workers in Western industrialised countries. In the Netherlands, about 15% of the working population report complaints in the neck, shoulders and arms [1] defined as pain, numbness, or tingling, resulting in loss of productivity, sick-leave or even disability. In 1998, about 8% of all Dutch employees were absent from work due to work-related musculoskeletal complaints, and 2% of the employee population was absent from work for more than four weeks [2]. These complaints impose a substantial economic burden in compensation costs, lost wages, and productivity. Apart from the individual suffering, the financial costs within member states of the European Union associated with musculoskeletal complaints are high [3].
Work-related musculoskeletal complaints are multifactorial in origin and involve biomechanical, psychosocial, and individual components [4–6]. As a consequence different intervention approaches exist. Most often interventions address alterations of the physical work environment by adjustments of the work station and/or education about working posture according to ergonomic principles [7–10]. There are several studies reporting on the effectiveness of ergonomic approaches [11, 12] and it is commonly accepted that properly designed work stations are prerequisites for healthy working. However, in spite of attention to ergonomics musculoskeletal complaints remain a considerable problem [13–15] and this is the rationale for the search for innovative interventions.
A relatively new intervention approach addressing neck-shoulder complaints is myofeedback training based on the Cinderella-hypothesis [16]. The Cinderella-hypothesis is one of the most influential hypotheses explaining the process of development and persistence of pain in low intensity jobs [17] like computer work, and states that lack of sufficient muscle relaxation is a crucial factor in this process. Continuous muscle activity, even at low intensity levels, may result in homeostatic disturbances of the activated motor units due to affected blood flow and removal of metabolites [17]. Several studies have found an association between absence of moments of complete muscle rest and myalgia, especially for the commonly affected descending part of the trapezius muscle (e.g. [18–20]). Warning subjects when their muscle relaxation is insufficient could thus contribute to recovery, and this is the rationale for the Cinderella-based myofeedback training. This approach is different from traditional myofeedback training in which feedback is provided when muscle activity exceeds a certain level thereby aiming at decreasing muscle activation (e.g. [21, 22]). As the Cinderella-hypothesis suggests however that muscle relaxation is more relevant than muscle activation, a myofeedback-based intervention aiming at increasing muscle relaxation may be more beneficial.
The Cinderella-based myofeedback system [23] consists of a harness incorporating dry surface electrodes and a feedback unit. The system is ambulant and subjects can wear the harness under their clothes during working days. The harness is connected to a feedback unit worn at the waist which provides feedback by means of vibration and a soft sound when muscle relaxation is insufficient. A feasibility study using this equipment for four weeks in a group reporting work-related neck-shoulder complaints resulted in significantly decreased levels of pain intensity and also changed muscle activation patterns. These effects were still at hand four weeks after the myofeedback training ended [23]. However, as the study did not contain a control group and only investigated the lasting effects of the intervention for a short follow-up period (4 weeks), further research is needed.
As proper ergonomics are indispensable for healthy working, the myofeedback training is preferably applied in combination with an intervention approach aimed at improving ergonomics. Thus, the present study aimed at investigating the immediate and lasting effects of Cinderella-based myofeedback training including ergonomic counselling, compared to ergonomic counselling alone, on pain intensity and disability in females with work-related neck-shoulder complaints. As interventions focusing on multiple factors have shown to be related to decreased incidence of complaints [24] it was hypothesised that 4-weeks myofeedback training including ergonomic counselling would be more effective in reducing pain intensity and disability than the intervention based on ergonomic counselling alone.
Methods and materials
Design and subjects
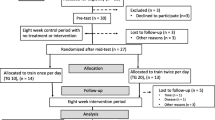
A randomized controlled trial was performed to assess the effect of 4-weeks Cinderella-based myofeedback training combined with ergonomic counselling (together referred to as Mfb), compared to ergonomic counselling alone (EC), on pain intensity and disability. Measurements were performed prior to intervention but before randomisation (Baseline), immediately after four weeks of intervention (T0), and at three (T3) and six (T6) months after the intervention.
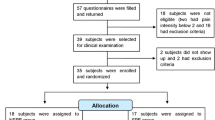
Participants were recruited in Sweden (area of Göteborg) and the Netherlands (area of Enschede) between March 2003 and June 2005. Computer workers like job counselors (Sweden) and (medical) secretaries (Sweden and the Netherlands) were approached by telephone and announcements, and volunteers were subsequently sent a screening questionnaire [25] which was developed within the EU-funded NEW project (Neuromuscular assessment in the Elderly Worker) [26]. Subjects eligible for participation were symptomatic female computer workers, predominantly over the age of 45 as the prevalence of complaints is especially high in this age category [27], working for at least 20 hours a week, and reporting perpetuating work-related musculoskeletal complaints in the neck and/or shoulder region for at least 30 days during the last year.
Subjects were excluded when they reported pain in more than 3 body regions, when they suffered from severe arthrosis or joint disorders, when they were using muscle relaxants, or when reporting other complaints in the upper extremity not related to (computer) work.
Power calculation, based on the results of Hermens and Hutten [23], indicated that at least 35 subjects should be included in each intervention group (estimated proportion of subjects showing an effect on pain intensity was set at 0.6 in the Mfb group and 0.2 in the EC group; 1−β = 0.90; α = .05). Block randomization was used to assign subjects to either Mfb or EC: When a new group of subjects started the intervention, half of them were assigned to Mfb and half of them were assigned to EC. The study was approved by the local Medical Ethics Committees and all participants gave their informed consent prior to participation.
Interventions
The interventions were provided by three different therapists: One physiotherapist in Sweden and two health scientists in the Netherlands. They were thoroughly trained and practiced together prior to the start of the study to ensure that they would provide as identical interventions as possible. The character of the intervention made blinding of the therapists and the subjects to the intervention impractical. To prevent from information bias, subjects were informed that the aim of the current study was to compare the effects of two interventions and that there was no evidence favouring one of these interventions.
Ergonomic counselling (EC)
Subjects received four weeks of intervention during which they kept a diary of activities and pain intensity scores. During the four weeks period they were visited weekly by their therapist. The first visit comprised an ergonomic workplace investigation by means of the risk inventory of Huppes et al. [28]. This checklist contains questions to evaluate work tasks, working hours, work load, work station, and working methods. Based on the outcome, possible improvements were discussed with the subject. With regard to the work station, the focus was primarily on modifying the existing work station rather than providing new equipment. The remaining visits were used to further discuss the ergonomic aspects, the consequences of possible ergonomic adjustments etc., according to a manual to guarantee a uniform intervention.
Myofeedback (Mfb)
Subjects randomized to the Mfb group received Cinderella-based myofeedback training on top of EC. A two-channel ambulant myofeedback system combined with a harness incorporating dry surface Electromyography (sEMG) electrodes to enable a stable recording of upper trapezius muscle activity was used. The harness was connected to a sEMG processing and storage device (see Picture 1).
The sEMG signal was amplified (15×), band pass filtered between 30 and 250 Hz, sampled at 512 Hz, digitized (22 bits ADC), and smooth rectified with removal of the low frequency components. Embedded software provided the detection and calculation of muscle rest, expressed as the sEMG parameter Relative Rest Time, which was defined as the percentage of time in which Root Mean Square was below a threshold (10 μV) for at least 0.12 s. This threshold was based on the noise level of the myofeedback system including mounted electrodes at the skin. Sensory feedback by means of vibration and a soft sound was provided after each 10 s interval when the relative duration of muscle relaxation in that particular interval was below 20%. The choice for a 10 s interval was based on the results of Voerman et al. [29], and the 20% threshold was chosen based on the work of Hägg and Åström [30]. Subjects were instructed that they should respond to the feedback by relaxation, which could be reached by slightly depressing the shoulders, or by sitting down quietly with the eyes closed, the hands in the lap while breathing deeply. Another relaxation strategy subjects were instructed was to maximally elevate the shoulders for three seconds to build up muscle tension and then to let loose this tension. This relaxation was anticipated to contribute to recovery of the Cinderella motor units. When there was no adequate response to the feedback, i.e. relaxation, the duration of the feedback signal progressively increased.
Immediately after Baseline, subjects assigned to the Mfb group were given the myofeedback device and they were explained the working mechanism and background of the myofeedback training. Subjects wore the system for four weeks, for at least eight hours a week (distributed over two hours a day and two days a week as a minimum) while performing their regular work. During the weekly visits the sEMG-data from last week were scrutinized and discussed to give the subject insight in their relaxation patterns and to identify possible situations of concern. This procedure was facilitated by means of the diary.
Assessment of pain intensity and disability
Pain intensity in the neck, shoulder (left and right), and upper back at time of the measurement was assessed by means of four Visual Analogue Scales [31]. Subjects were instructed to rate their subjectively experienced level of pain intensity at that moment for each body region. The Visual Analogue Scale consists of a 10 cm horizontal line with ‘no discomfort at all' at the left and ‘as much discomfort as possible' at the right endpoints of the line. Psychometric properties of the Visual Analogue Scale have been shown to be sufficient [32–34].
The level of subjectively experienced disability was assessed with the Pain Disability Index, a self-rating scale that measures the impact of pain on the abilities to participate in life activities [35]. The Pain Disability Index contains 7 items, one for each domain, i.e. (1) family and home responsibilities, (2) recreation (hobbies, sports, and leisure time activities), (3) social activity (participation with friends and acquaintances), (4) occupation (activities partly or directly related to working), (5) sexual behavior (frequency and quality of sex life), (6) self care (personal maintenance and independent daily living), and (7) life-support activity (basic life-supporting behaviors). Answers were provided on a categorical 11-points scale with ‘not disabled’ and ‘fully disabled’ at the extremes. In a chronic pain population, psychometric properties of the Pain Disability Index appeared to be sufficient [36].
Analysis
Data inspection showed non-normal distributions for all of the variables, and data were therefore log transformed, enabling parametric analyses. Analyses were performed both on the group as well as the individual level.
For each subject, VAS scores for the neck, left shoulder, right shoulder, and upper back were summed and averaged resulting in a combined neck-shoulder pain intensity score. Differences between the two interventions, i.e. Mfb and EC, for VAS and the Pain Disability Index were investigated using a linear mixed-model analysis technique for repeated measurements. The following variables were included in the model as fixed factors: Time of measurement (i.e. Baseline, T0, T3, and T6), intervention type (i.e. Mfb and EC), and study group (i.e. Sweden and the Netherlands), including two-way interactions. The factor study group comprises variance due to possible (socio)demographic differences as well as variance caused by the different therapists, organizations, and job characteristics in the two countries. The factor subject was included in the model as a random factor. Paired and independent samples t-tests were used for Post Hoc analysis.
At the individual level the percentages of subjects improving and the odds for improvement in both intervention groups were investigated. First, individual differences were calculated between Baseline and T0, Baseline and T3, and Baseline and T6 for pain intensity in the neck-shoulder region (i.e. the averaged score on the VAS for neck, left and right shoulders, and upper back) and Pain Disability Index. These differences were then dichotomized into ‘clinically relevant improvement’ or ‘equal/deteriorated.’ For the Visual Analogue Scale the cut-off point for a clinically relevant improvement was defined at 13 mm which corresponds to the upper limit of the confidence interval of clinically relevant changes in Visual Analogue Scale scores in acute and non-acute pain patients as reported by Kelly in 2001 [37]. This cut-off point was also the result of the study of Todd [34]. Cut-off points for clinically significant changes in the Pain Disability Index scores have not been provided in literature. For a comparable measure, the Neck Disability Index which is a 10 items scale with 6 answering options resulting in scores varying from 0 to 50, the cut-off point was set at 5 which is 10% of the maximum score [38]. Using this as a starting point, a clinically relevant change was defined as a change of ≥10% of the maximum score of 70 of the Pain Disability Index, i.e. ≥7 units of the Pain Disability Index score.
Logistic regression analyses providing Odds Ratios were performed to investigate whether the two intervention groups differed in terms of chances for clinically relevant improvements in pain intensity and disability. Three different models were investigated: Model I represents the crude Odds Ratio describing only the relationship between intervention type and odds for improvement without adjustment for confounding factors. The factors study group and baseline pain intensity/baseline disability were assumed potentially confounding factors. To correct for these factors, two additional models were built as extensions of Model I: Model II incorporates study group as confounding factor, and Model III is an extension of Model II incorporating also the factor baseline pain intensity/baseline disability level. For Models II and III interaction effects were additionally included in the analysis, to study effect modification, but these remained only included when significant. −2 Log Likelihood tests were used to select the best model. Odds Ratios including 95% Confidence Intervals were calculated and presented for each of the models.
Statistical Package for Social Sciences 11.5 was used for statistical testing and alpha was set at .05 for statistical significance.
Results
Subjects
Seventy-nine female computer workers with neck-shoulder complaints were included in this study: Forty-two subjects were assigned to the Mfb group and 37 to the EC group. Mean age was 52.0 (SD 5.8 years) in the Mfb group and 50.7 (SD 5.5) years in the EC group. Mean duration (days between Baseline and T0) of the interventions was 37 (SD 8) days for the Mfb group and 36 (SD 7) days for the EC group. Forty-one out of the 79 subjects were recruited in Sweden and the remaining 38 in the Netherlands. The number of subjects at Baseline, T0, T3, and T6 and the number of drop-outs are shown in Diagram 1.
Drop-outs did not differ in age, weight, height, BMI, and pain intensity scores (Visual Analogue Scale), and disability (Pain Disability Index) from those fulfilling the intervention (p > .08).
Table 1 provides an overview of sociodemographic characteristics of the subjects in the Mfb and EC groups. Thirty-eight subjects reported complaints in both the neck and shoulder, while 41 subjects reported complaints either in the neck or in the shoulder at the time of recruitment. Comparison of the characteristics between the Mfb and EC groups indicated that subjects assigned to the Mfb group reported more years within the same job compared to the EC group (p < .05).
Analysis at group level
Pain intensity
Baseline (geometric) mean VAS scores for each region separately were 27 mm (neck), 15 mm (left shoulder), 14 mm (right shoulder), and 13 mm (upper back) in the Mfb group and 24, 14, 19, and 18 mm in the EC group respectively.
Figure 1 shows a box plot of the VAS score in the neck-shoulder region at Baseline, T0, T3, and T6 for the Mfb and the EC group. A clear decrease was observed at T0, T3, and T6 compared to Baseline, although at T6 pain intensity seemed to increase slightly in both groups.
Mixed linear modelling showed that pain intensity in the neck-shoulder region significantly changed over time (F = 12.08, p ≤ .01), without additional effects for the type of the intervention (F = 1.54, p = 0.22), study group (F = .48, p = .49), or interaction effects (F ≤ .87, p ≥ .35). Post Hoc comparisons revealed that the VAS score was significantly reduced at T0 (t = 4.37, p < .01), T3 (t = 5.10, p < .01), and T6 (t = 3.54, p < .01) compared to Baseline but also the reduction between T0 and T3 was significant (t = 2.85, p = .01).
Disability
Figure 2 shows a box plot of the Pain Disability Index score at Baseline, T0, T3, and T6 for the Mfb and the EC group. A comparable pattern to what was observed for pain intensity was found, with decreased disability levels at T0, T3, and T6 compared to Baseline.
Disability levels significantly changed over time (F = 17.68, p < .01) and were significantly different between the two study groups (i.e. Sweden and the Netherlands) (F = 5.30, p = .02). No additional effects were found for intervention type (F = .86, p = .35) nor the interaction terms (F ≤ 1.97, p ≥ .12). Post Hoc comparisons showed that subjects in the Swedish study group had lower Baseline values and reported reductions in disability only between Baseline and T0 (t = 2.20, p = .04) with a trend for reductions at T3 (t = 1.89, p = .07) and T6 (t = 1.81, p = .08). Subjects in the Dutch study group showed a significant decrease at T0 (t = 3.26, p < .01), T3 (t = 3.58, p < .01), and T6 (t = 3.51, p < .01) compared to Baseline.
Analysis at the individual level
Pain intensity
Figure 3 gives an overview of the percentage of subjects in the Mfb and EC groups showing an improvement in pain intensity in the neck-shoulder region. About half of the subjects showed a clinically relevant improvement in pain intensity in the neck-shoulder region. Slightly more subjects in the Mfb group showed improvements compared to the subjects in the EC group immediately after the intervention period (T0) and at 6 months follow-up (T6).
Crude Odds Ratios (Model I) for improvement showed higher odds for clinically relevant improvement in the Mfb group at T0 and T6 compared to Baseline, while between T3 and Baseline subjects assigned to EC were more likely to show improvements (see Table 2). However, Odds Ratios were not significant (p ≥ .36) also not when corrected for potential confounding factors (p > .19). −2 Log Likelihood tests indicated that Model III, adjusting for the factors study group and baseline pain intensity/disability level, superimposed the Models I and II (−2 LL; p < .05). As no significant interaction effects were found (p > .08) these were excluded from the final models as presented in Table 2.
Disability
An overview of the percentage of subjects in the Mfb and EC groups showing an improvement in disability is provided in Fig. 4.
Immediately after the intervention period about twice as many of the subjects in the Mfb group showed clinically relevant improvements in disability compared to the EC group. This share of subjects increased somewhat in both groups after three months and then showed a small decline after six months where about one third of the subjects of the EC group and half of the Mfb group showed clinically relevant improvements in disability.
Subjects assigned to the Mfb group had higher odds for improvement in disability at T0, T3, and T6: At T3, the odds for improvement in disability was 2.77 times higher in the Mfb group compared to the EC group which was significant (Model I; 95% CI 1.00–7.65; p = .05). When corrected for confounding variables, however, Odds Ratios for improvement were still higher for the Mfb group compared to the EC group, but this was not significant (p ≥ .057) except for Model II for changes between Baseline and T3 (p = .04). Baseline disability levels significantly affected Odds Ratios: Model III was generally better than the models I and II (−2 LL; p < .05). As no significant interaction effects were found (p > .08) these were excluded from the final models as presented in Table 3.
Discussion
This randomised controlled trial investigated the effects of 4-weeks ambulant myofeedback training combined with ergonomic counselling in subjects with work-related neck-shoulder complaints relative to ergonomic counselling alone, on pain intensity and disability. The effects were evaluated immediately after the interventions, and at three and six months follow-up. Mean pain intensity and disability levels significantly reduced after both interventions (i.e. Mfb and EC). The effects were clinically relevant in a large part of the subjects: About 30–50% of the subjects showed clinically relevant improvements in pain intensity and/or disability. No difference was found for the effect of the intervention on outcome and after correction for confounding factors subjects in both intervention groups did not differ with regard to chances for clinically relevant improvements in pain intensity and disability.
Several studies have shown the beneficial effect of myofeedback training on pain reduction [21, 39–43] although Faucett and colleagues [22] reported changes in muscle activity rather than changes in pain intensity. The feedback approach used in these studies is different from the Cinderella-based myofeedback approach in that the traditional feedback method provides feedback when muscle activation is too high [21, 22, 42, 44–47], rather than when the time the muscle has relaxed is too short [23]. Two previous studies applying the Cinderella-based myofeedback training in subjects with work-related complaints [23] and subjects with a whiplash associated disorder [48] reported reduced pain intensity and disability levels. Compared to these studies, baseline pain intensity values were generally lower and the cut-off points for clinically relevant changes were set to higher levels in the current study, but the results indicate a comparable percentage of subjects reporting clinically significant reductions in pain intensity, i.e. between 35 and 50% of the subjects. This consistency in results adds to evidence for the effectiveness of (Cinderella-based) myofeedback training on pain intensity and disability in musculoskeletal neck-shoulder complaints.
In line with existing literature (e.g. [8, 10, 49, 50]) also subjects in the ergonomic counselling group reported reduced pain intensity and disability. It was however hypothesised that a treatment approach including both myofeedback training and ergonomic counselling (Mfb) would be more effective than treatment comprising only ergonomic counselling (EC) as interventions focusing on multiple factors have shown to be related to decreased incidence of complaints [24]. In the current study the two types of interventions did not differ in terms of outcome. This is in line with findings of other studies (e.g. [8, 10, 51–53]) that concluded that occupational interventions have generally comparable effects, although these studies did not include a myofeedback intervention. Newton-John and others [43] compared myofeedback with cognitive-behavioural therapy and a waiting list control group and found that both interventions showed favourable outcome in terms of pain intensity and disability compared to the waiting list control group without a difference between the two interventions.
There are possible explanations for the absence of differences between the two groups. One concerns the presence of subgroups in which the intervention is beneficial. Results showed that the effect is clinically relevant in about 30–50% of the subjects. Main question to be addressed here is whether, and how, these subjects can be characterised in terms of cognitive-behavioural characteristics and whether this characterisation can contribute to predict outcome of the intervention. This could substantially improve the efficiency and effectiveness of the interventions. Further, differences between the two groups may have been masked by using rather generic outcome measures. For instance, coping and patient-rated parameters may better represent the difference in outcome between different kinds of interventions [54]. Investigation into the specific working mechanisms of both interventions could clarify this. Finally, initial VAS and disability levels were low in both the Mfb and the EC group, especially in the study group from Sweden. This results in a smaller potential for improvement (floor effect) and as a result a smaller chance for finding differences between the Mfb and EC groups.
Methodological considerations
This study did not include a non-intervention or placebo control group (for instance randomly administered feedback) which makes it hard to control for non-specific effects like regression to the mean or the Hawthorne effect [55]. This effect was already described in 1933 by Mayo, and is reported as a significant positive effect without causal basis in the theoretical motivation for the intervention, but is related to the effect on the participants knowing themselves to be studied in connection with the outcomes measured. An argument against such effect is that although it might occur in connection with the intervention (i.e. at T0) it is not likely that this effect would remain [56] after three to six months. In addition, the study population also contained subjects with chronic complaints (i.e. duration >6 months) who received a variety of treatments in the past, which were not successful. It is likely to expect that any non-specific effects of treatment would already have occurred during past treatments and that this effect in the current study would thus be small. Furthermore, results from previous studies learned that pain reduction in myofeedback-trained subjects were higher compared to a wait-list control group [43], a no intervention group [46], or subjects receiving a placebo [57]. Furthermore, an attention-only group showed no changed outcome in terms of disability and pain intensity [58].
The present study included a rather specific subject population: Participants were females, predominantly over the age of 45, still at work, and characterised by relatively low pain intensity and disability levels. Interpretation and extrapolation of results to other populations therefore requires caution, but as comparable effects of Cinderella-based myofeedback training have also been shown in mixed, younger subject populations [23, 48] and in a sample of patients who were on sick leave because of their neck-shoulder complaints [48], generalisation of findings might be legitimate. The subjects were selected based on self-reported complaints rather than a clinical evaluation. In a previous study [60] with female computer users above the age of 45, applying the same inclusion criteria as the present study, it was found that in subjects with neck-shoulder complaints the following clinical diagnoses were most prevalent: Trapezius myalgia (38%), tension neck syndrome (17%), and cervicalgia (17%). These diagnoses were found in 60% of the subjects reporting complaints. There were cases with supraspinatus tendinitis, frozen shoulder, and biceps tendinitis, but these were less common. This general pattern of clinical signs is likely to be at hand also in the present study. It could be hypothesised that myofeedback may be particularly relevant and helpful in cases with muscular pain syndromes.
Despite extensive standardisations, the recruitment of subjects in two different study groups (Sweden and the Netherlands) resulted in heterogeneity of the subject population with regard to age, working hours, seniority, and working posture. To correct for this, the factor study group was considered a confounder needed to control for during analysis. This reduced the power of the study. An additional likely confounding factor is the compliance of the patient and therapist to the intervention. This is an often uncontrolled and thus potentially confounding factor in occupational intervention studies [59] and it is known that changes in knowledge and skills do not necessarily result in a behavioural change. In the Mfb group, the compliance was partly controlled as the number of hours the system was worn was recorded by the system itself, but the compliance to ergonomic knowledge and skills is hard to register objectively. This definitely is a challenge in future occupational intervention studies.
The drop-out rate in the Mfb group was higher than in the EC group (i.e. nine compared to five), which was probably related to the myofeedback system itself. Some subjects found the system inconvenient and disturbing in daily working activities. This may have suppressed the effect of the intervention. Improvement of the current device in terms of usability is therefore required to optimise the myofeedback training.
Conclusions
Four-weeks of intervention significantly reduced pain intensity and disability, and this effect remained after three and six months follow-up. Myofeedback training combined with ergonomic counselling is thus beneficial for female computer workers over the age of 45, reporting pain and disability in the neck-shoulder region but no evidence was found favouring myofeedback training combined with ergonomic counselling over ergonomic counselling alone. Future research may aim at identifying possible subgroups of patients in which the interventions are especially beneficial. This may enhance the efficiency and the effectiveness of the interventions. Finally, as non-specific effects may have interfered with outcome, future studies could include a placebo control group for more insight in the specific effects of ambulant myofeedback training combined with ergonomic counselling.
References
Blatter B, Houtman I, van den Bossche S, Kraan K, van den Heuvel S. Gezondheidsschade en kosten als gevolg van RSI en psychosociale arbeidsbelasting in Nederland [Health damage and costs of RSI and psychosocial work load in the Netherlands]. TNO rapport, 2005.
Bongers PM, Kremer AM, ter Laak J. Are psychosocial factors, risk factors for symptoms and signs of the shoulder, elbow, or hand/wrist? A review of the epidemiological literature. Am J Ind Med 2002;41(5):315–42.
Buckle PW, Devereux JJ. The nature of work-related neck and upper limb musculoskeletal disorders. Appl Ergon 2002;33(3):207–17.
Kamwendo K, Linton SJ, Moritz U. Neck and shoulder disorders in medical secretaries. Part I. Pain prevalence and risk factors. Scand J Rehabil Med 1991;23(3):127–33.
Huang GD, Feuerstein M, Sauter SL. Occupational stress and work-related upper extremity disorders: concepts and models. Am J Ind Med 2002;41(5):298–314.
Andersen JH, Kaergaard A, Mikkelsen S, Jensen UF, Frost P, Bonde JP, Fallentin N, Thomsen JF. Risk factors in the onset of neck/shoulder pain in a prospective study of workers in industrial and service companies. Occup Environ Med 2003;60(9):649–54.
Linton SJ, van Tulder MW. Preventive interventions for back and neck pain problems: what is the evidence? Spine 2001;26(7):778–87.
Ketola R, Toivonen R, Hakkanen M, Luukkonen R, Takala EP, Viikari-Juntura E. Effects of ergonomic intervention in work with video display units. Scand J Work Environ Health 2002;28(1):18–24.
Horgen G, Aarås A, Dainoff MJ, Konarska M, Thoresen M, Cohen BG. A cross-country comparison of short- and long-term effects of an ergonomic intervention on musculoskeletal discomfort, eyestrain and psychosocial stress in VDT operators: selected aspects of the international project. Int J Occup Saf Ergon 2005;11(1):77–92.
Feuerstein M, Nicholas RA, Huang GD, Dimberg L, Ali D, Rogers H. Job stress management and ergonomic intervention for work-related upper extremity symptoms. Appl Ergon 2004;35(6):565–74.
Dainoff MJ, Aarås A, Horgen G, Konarska M, Larsen S, Thoresen M, Cohen BG. The effect of an ergonomic intervention on musculoskeletal, psychosocial and visual strain of VDT entry work: organization and methodology of the international study. Int J Occup Saf Ergon 2005;11(1):9–23.
Ketola R, Toivonen R, Hakkanen M, Luukkonen R, Takala EP, Viikari-Juntura E. Effects of ergonomic intervention in work with video display units. Scand J Work Environ Health 2002;28(1):18–24.
Westgaard RH, Winkel J. Ergonomic intervention research for improved musculoskeletal health: a critical review. Int J Ind Ergon 1997;20:463–500.
Brandt LP, Andersen JH, Lassen CF, Kryger A, Overgaard E, Vilstrup I, Mikkelsen S. Neck and shoulder symptoms and disorders among Danish computer workers. Scand J Work Environ Health 2004;30(5):399–409.
Ekman A, Andersson A, Hagberg M, Hjelm EW. Gender differences in musculoskeletal health of computer and mouse users in the Swedish workforce. Occup Med (Lond) 2000;50(8):608–13.
Hägg GM. Static work loads and occupational myalgia- a new explanation model. Anderson PA, Hobart DJ, Dainoff JVe. Electromyographical Electromyography. Elsevier Science Publishers B.V. (Biomedical Division); 1991. p. 141–3.
Visser B, van Dieën JH. Pathophysiology of upper extremity muscle disorders. J Electromyogr Kinesiol 2006;16(1):1–16.
Sandsjö L, Melin B, Rissén D, Dohns I, Lundberg U. Trapezius muscle activity, neck and shoulder pain, and subjective experiences during monotonous work in women. Eur J Appl Physiol 2000;83(2–3):235–8.
Veiersted KB, Westgaard RH, Andersen P. Electromyographic evaluation of muscular work pattern as a predictor of trapezius myalgia. Scand J Work Environ Health 1993;19(4):284–90.
Lundberg U. Stress responses in low-status jobs and their relationship to health risks: musculoskeletal disorders. Ann N Y Acad Sci 1999;896:162–72.
Nord S, Ettare D, Drew D, Hodge S. Muscle learning therapy—efficacy of a biofeedback based protocol in treating work-related upper extremity disorders. J Occup Rehabil 2001;11(1):23–31.
Faucett J, Garry M, Nadler D, Ettare D. A test of two training interventions to prevent work-related musculoskeletal disorders of the upper extremity. Appl Ergon 2002;33(4):337–47.
Hermens HJ, Hutten MMR. Muscle actvation in chronic pain: its treatment using a new approach of myofeedback. Int J Ind Ergon 2002;30:325–36.
Lincoln AE, Vernick JS, Ogaitis S, Smith GS, Mitchell CS, Agnew J. Interventions for the primary prevention of work-related carpal tunnel syndrome. Am J Prev Med 2000;18(4 Suppl):37–50.
Sandsjö L, Larsman P, Vollenbroek-Hutten MMR, Läubli T, Juul-Kristensen B, Klipstein A, Hermens H, Søgaard K. Comparative assessment of study groups of elderly female computer users from four European countries: questionnaires used in the NEW study. Eur J Appl Physiol 2006;96(2):122–6.
Sjøgaard G, Søgaard K, Hermens HJ, Sandsjö L, Läubli T, Thorn S, Vollenbroek-Hutten MM, Sell L, Christensen H, Klipstein A, Kadefors R, Merletti R. Neuromuscular assessment in elderly workers with and without work related shoulder/neck trouble: the NEW-study design and physiological findings. Eur J Appl Physiol 2006;96(2):110–21.
Guez M. Chronic neck pain. An epidemiological, psychological and SPECT study with emphasis on whiplash-associated disorders. Acta Orthop Suppl 2006;77(320):1, 3–33.
Huppes G, Peereboom KJ, Schreibers KBJ. Checklist RSI bij beeldschermwerk: preventie en reintegratie [Checklist RSI in computer work: Prevention and rehabilitation]. Zeist: Kerckebosch, 1997.
Voerman GE, Sandsjö L, Vollenbroek-Hutten MM, Groothuis-Oudshoorn CG, Hermens HJ. The influence of different intermittent myofeedback training schedules on learning relaxation of the trapezius muscle while performing a gross-motor task. Eur J Appl Physiol 2004;93(1–2):57–64.
Hägg GM, Åström A. Load pattern and pressure pain threshold in the upper trapezius muscle and psychosocial factors in medical secretaries with and without shoulder/neck disorders. Int Arch Occup Environ Health 1997;69(6):423–32.
Gift A. Visual Analogue Scales: Measurement of subjective phenomena. Nurs Res 38:286–8.
Huskisson EC. Measurement of pain. Lancet 1974;2(7889):1127–31.
Todd KH. Clinical versus statistical significance in the assessment of pain relief. Ann Emerg Med 1996;27(4):439–41.
Todd KH, Funk KG, Funk JP, Bonacci R. Clinical significance of reported changes in pain severity. Ann Emerg Med 1996;27(4):485–9.
Pollard CA. Preliminary validity study of the pain disability index. Percept Mot Skills 1984;59(3):974.
Tait RC, Chibnall JT, Krause S. The Pain Disability Index: psychometric properties. Pain 1990;40(2):171–82.
Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J 2001;18(3):205–7.
Stratford PW, Riddle DL, Binkley JM. Using the Neck Disability Index to make decisions concerning individual patients. Physiother Can 107–12.
Flor H, Birbaumer N. Comparison of the efficacy of electromyographic biofeedback, cognitive-behavioral therapy, and conservative medical interventions in the treatment of chronic musculoskeletal pain. J Consult Clin Psychol 1993;61(4):653–8.
Sarnoch H, Adler F, Scholz OB. Relevance of muscular sensitivity, muscular activity, and cognitive variables for pain reduction associated with EMG biofeedback in fibromyalgia. Percept Mot Skills 1997;84 (3 Pt 1):1043–50.
Stuckey SJ, Jacobs A, Goldfarb J. EMG biofeedback training, relaxation training, and placebo for the relief of chronic back pain. Percept Mot Skills 1986;63(3):1023–36.
Middaugh SJ, Woods SE, Kee WG, Harden RN, Peters JR. Biofeedback-assisted relaxation training for the aging chronic pain patient. Biofeedback Self Regul 1991;16(4):361–77.
Newton-John TR, Spence SH, Schotte D. Cognitive-behavioural therapy versus EMG biofeedback in the treatment of chronic low back pain. Behav Res Ther 1995;33(6):691–7.
Madeleine P, Vedsted P, Blangsted AK, Sjøgaard G, Søgaard K. Effects of electromyographic and mechanomyographic biofeedback on upper trapezius muscle activity during standardized computer work. Ergonomics 2006;49(10):921–33.
Peper, E, Wilson, VS, Taylor, W, Pierce, A, Bender, K, Tibbetts, V. Repetitive Strain Injury. Prevent computer user injury with biofeedback: Assessment and training protocol [Web Page]. Available at http://www.bfe.org/protocol/pro09eng.htm (accessed 2004).
Spence SH, Sharpe L, Newton-John T, Champion D. Effect of EMG biofeedback compared to applied relaxation training with chronic, upper extremity cumulative trauma disorders. Pain 1995;63(2):199–206.
Cohen SL, Richardson J, Klebez J, Febbo S, Tucker D. EMG biofeedback: the effects of CRF, FR, VR, FI, and VI schedules of reinforcement on the acquisition and extinction of increases in forearm muscle tension. Appl Psychophysiol Biofeedback 2001;26(3):179–94.
Voerman GE, Vollenbroek-Hutten MMR, Hermens HJ. Effects of ambulant myofeedback training in pain, disability, and muscle activation patterns in chronic Whiplash patients. Clin J Pain 2006;22(7):656–663.
Robertson MM, O'Neill MJ. Reducing musculoskeletal discomfort: effects of an office ergonomics workplace and training intervention. Int J Occup Saf Ergon 2003;9(4):491–502.
Dainoff MJ, Aaras A, Horgen G, Konarska M, Larsen S, Thoresen M, Cohen BG. The effect of an ergonomic intervention on musculoskeletal, psychosocial and visual strain of VDT entry work: organization and methodology of the international study. Int J Occup Saf Ergon 2005;11(1):9–23.
Waling K, Sundelin G, Ahlgren C, Jarvholm B. Perceived pain before and after three exercise programs—a controlled clinical trial of women with work-related trapezius myalgia. Pain 2000;85(1–2):201–7.
Waling K, Jarvholm B, Sundelin G. Effects of training on female trapezius myalgia: An intervention study with a 3-year follow-up period. Spine 2002;27(8):789–96.
Ekberg K, Bjorkqvist B, Malm P, Bjerre-Kiely B, Axelson O. Controlled two year follow up of rehabilitation for disorders in the neck and shoulders. Occup Environ Med 1994;51(12):833–8.
Taimela S, Takala EP, Asklof T, Seppala K, Parviainen S. Active treatment of chronic neck pain: a prospective randomized intervention. Spine 2000;25(8):1021–7.
Mayo E. The human problems of industrial civilization. New York: MacMillan; 1933.
Spence SH. Cognitive-behavior therapy in the management of chronic, occupational pain of the upper limbs. Behav Res Ther 1989;27(4):435–46.
Medlicott MS, Harris SR. A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther 2006;86(7):955–73.
Nicholas MK, Wilson PH, Goyen J. Comparison of cognitive-behavioral group treatment and an alternative non-psychological treatment for chronic low back pain. Pain 1992;48(3):339–47.
Zwerling C, Daltroy LH, Fine LJ, Johnston JJ, Melius J, Silverstein BA. Design and conduct of occupational injury intervention studies: a review of evaluation strategies. Am J Ind Med 1997;32(2):164–79.
Juul-Kristensen B, Kadefors R, Hansen K, Byström P, Sandsjö L, Sjøgaard G. Clinical signs and physical function in neck and upper extremities among elderly female computer users. The NEW-study. Eur J Appl Physiol 2006;96:136–145.
Acknowledgements
This work was undertaken within the project ‘Neuromuscular Assessment of the Elderly Worker (NEW)', with partial financial support from the EC within the RTD action QRLT 2000 00139, and by funding of the exchange visits by NWO-Nl and the Swedish Research Council. The authors would like to thank Lena Grundell and Linda Oostendorp for their valuable contribution to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Voerman, G.E., Sandsjö, L., Vollenbroek-Hutten, M.M.R. et al. Effects of Ambulant Myofeedback Training and Ergonomic Counselling in Female Computer Workers with Work-Related Neck-Shoulder Complaints: A Randomized Controlled Trial. J Occup Rehabil 17, 137–152 (2007). https://doi.org/10.1007/s10926-007-9066-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-007-9066-3